
UC Irvine faculty in psychiatry and computer science are collaborating with Asahi Breweries to develop a smartwatch-based application for diagnosing and predicting stress and depression.
When Asahi Breweries wanted to develop a smartwatch app for monitoring intoxication, the company collaborated with Sergio Gago-Masague, a computer science professor at UC Irvine. He helped design predictive algorithms that leverage data from a commercial smartwatch — motion, location, and heart and respiration rates — to predict a user’s blood alcohol concentration.
When Asahi wanted to develop a similar app for monitoring stress levels, Gago-Masague reached out to a colleague in the School of Medicine, Firoza Mamdani, PhD. As an assistant researcher of psychiatry and human behavior, Mamdani has a background in studying stress and depression and identifying biomarkers.
“I’m very excited about this project,” says Mamdani, who recruited other colleagues in the Department of Psychiatry & Human Behavior to join her, including psychiatrist Gemma Espejo, MD, and associate researcher and geneticist Pedro Adolfo Sequeira, PhD. “This allows computer science and psychiatry to actually work together.”
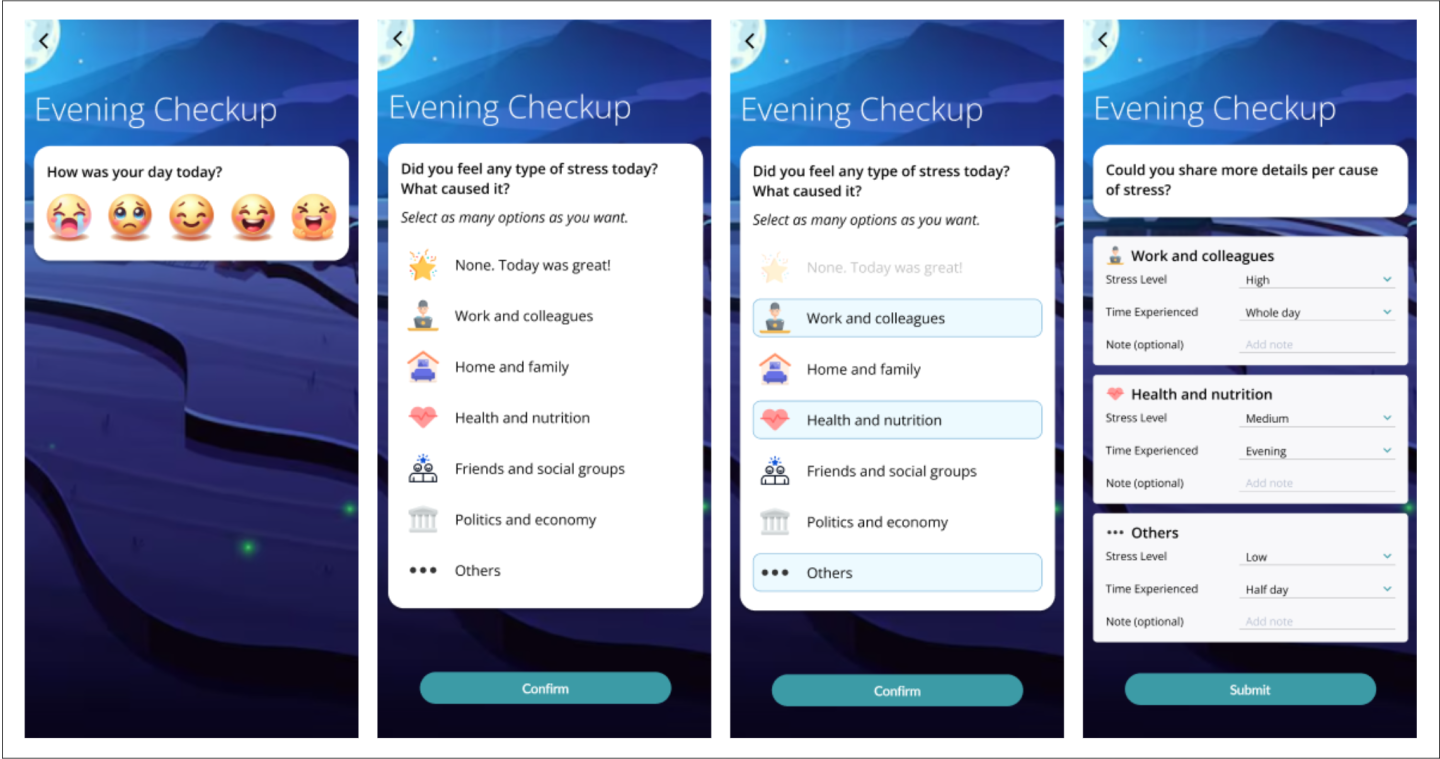
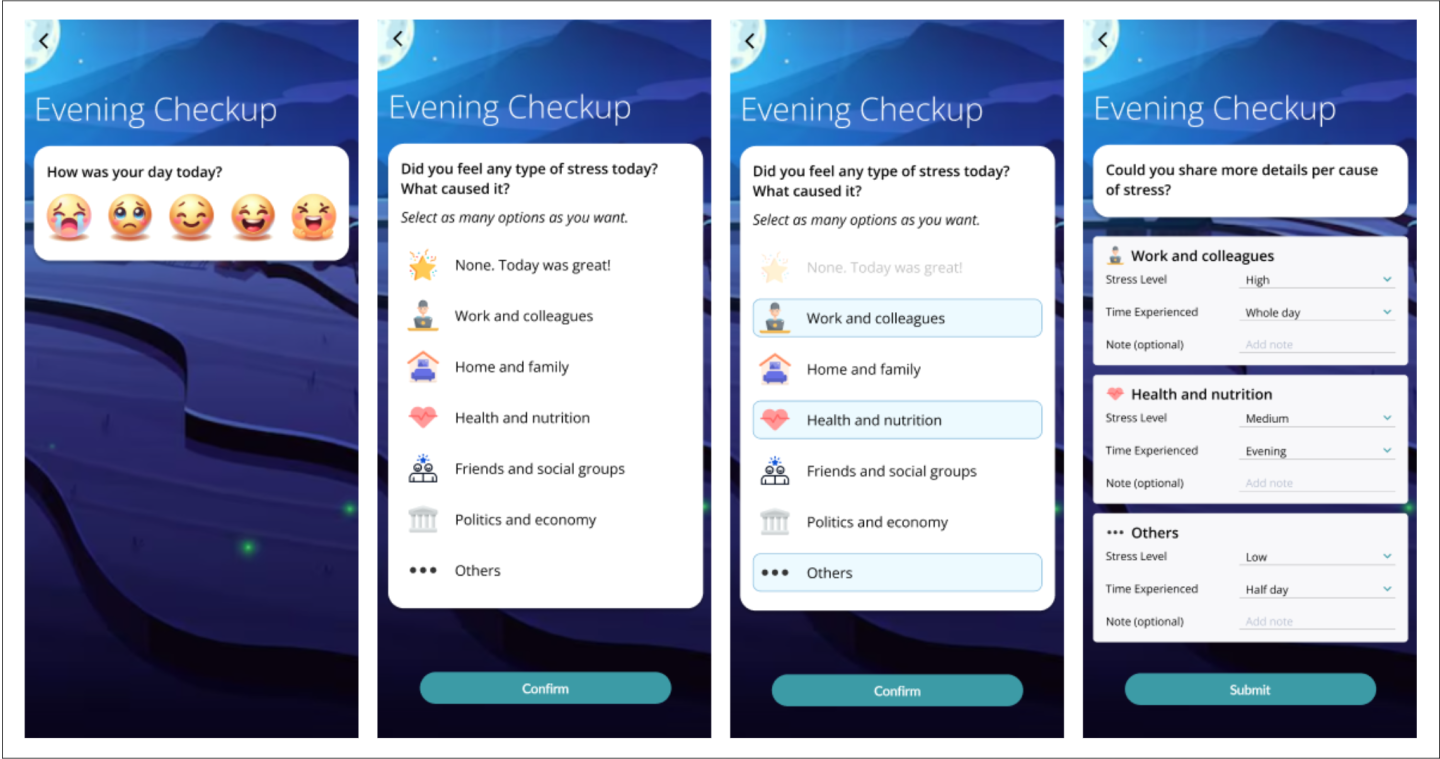
Dubbed “StressDX,” or stress diagnosis, the project aims to develop AI-driven stress prediction models using real-world, multimodal health data. “If we know when someone will experience high levels of stress,” says Mamdani, “we can intervene before it spirals out of control or leads to depression.”
Expertise for Training
The first phase of the project took place in Japan at Asahi, with researchers validating models using wearable data from a healthy population. Phase 2 is based out of UC Irvine, with Mamdani recruiting a cohort of around 40 participants for a six-month study.
“In phase 2, we are extending the models by training them on a richer dataset that includes wearable signals, psychological assessments and biological stress markers — such as cortisol, telomere length and gene expression — collected from patients diagnosed with major depressive disorder (MDD),” explains Gago-Masague. Although gene expression and other molecular markers aren’t practical features for real-time tracking, they enhance training for the models. “These biomarkers help us validate and better understand the physiological underpinnings of stress.”
Mamdani has extensive expertise in this area. Named an emerging innovator in 2024 for groundbreaking work in genetics and neuropsychiatric research, she has conducted studies on brain and blood-based biomarkers for suicide in depression. “We observe suicide-related gene expression patterns related to stress response, accelerated cellular aging, immune dysfunction and mitochondrial dysfunction,” she says. She and Sequeira are also in the middle of a three-year, $1.5 million grant focused on identifying brain-relevant blood-based biomarkers for suicide in MDD. “We’re performing a clinical study to look at people when they’re highly suicidal and then again when they’re getting better, so we can get more precise biomarkers.”
This work aligns well with the StressDX project, which builds on Mamdani’s expertise in translational research and leverages her experience in recruiting depressed patients. “Asahi did their assessment of stress in a control population, so we’re expecting those markers to be heightened in a depressed population,” she says. Identifying more precise markers for stress can help researchers determine which sensor data might serve as a predictor for stress and depression. “We want to see how saliva or hair cortisol measurements, and biological markers, correlate with measures of stress,” she explains. “If they can be used to predict stress, how well do they also correlate with data coming from a smartwatch, such as heartbeat, respiration, oxygen and activity levels, and hours of sleep?”
Just-in-Time Interventions
The goal is to support just-in-time interventions — perhaps a meditation notification, exercise reminder, or, if the issue persists, an alert to contact a psychologist or psychiatrist.
“We know people are not always as honest as they could be when talking to a clinician, because there’s a lot of shame, stigma and judgment still attached with mental health,” says Mamdani. “But sensor data isn’t going to lie; it’s measuring what’s actually happening in your body.”
Asahi hopes to use the app to help employees better monitor and manage their stress, but Mamdani says this could be applied in other settings as well. “Nurses could wear these, or we could expand it beyond employee well-being to help students,” she says. “Implementing computer science methods like machine learning and having predictive modeling can help prevent depression, suicide, and other psychiatric conditions or diseases.”
Gago-Masague is similarly pleased with the cross-disciplinary collaboration. “Working with Firoza and the School of Medicine team has opened new pathways, especially in integrating digital phenotyping with clinical biomarkers,” he says. “This fusion of technical and clinical insight is guiding our thinking around just-in-time interventions and broader healthcare applications. The synergy enables us to work toward human-centered, clinically relevant AI solutions.”